Clinical Trial Management: Houston, We Have a Problem

Publication Date: April 2015 / Download as PDF
Author: Reginald Exume
In the management of clinical trials, whether they be local, international, multi-site, simple or complex, a variety of situations can (or should I say will) occur that will have you saying “Houston, we have a problem!” These complications may be related to an issue at the clinical site itself, within the CRO or at the Sponsor level, but could also be caused by the study protocol or the investigational drug itself. This white paper will present a methodology to optimize clinical trial management by using best practices, as well as how to avoid and resolve problematic situations that may arise throughout the trial.
Optimizing management of clinical trials
Let us begin by considering the following two statements:
- Statement 1: The three main goals in the management of clinical trials are: 1) to reach the trial objective(s), 2) to respect the budget and study timelines and 3) to minimize the risks that can derail the first two goals.
- Statement 2: The Project Management Institute (PMI) defines a project as a temporary group of activities designed to produce a unique result[1]. Each clinical trial (i.e. project) is therefore considered “temporary” (due to a defined duration), and is “unique” because it is not a routine operation and involves the collaboration of different groups of people to achieve a well-defined goal.
In order to begin optimizing clinical trial management, an organization should aim to apply what is called the Project Management Body of Knowledge (commonly known as the PMBOK[2]), which consists of best practices in project management methods to ensure the success of a project from start to finish.
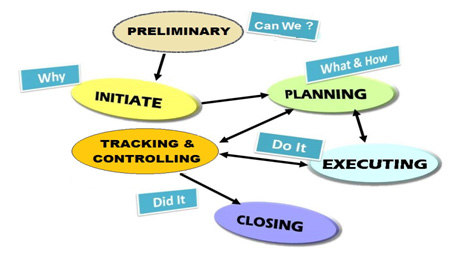
Utilizing the PMBOK principles, clinical trial management can be categorized into the following six stages:
- Preliminary stage:
This is where you must evaluate and assess if a clinical trial is feasible based on the investigational product (IP) and the scope of the study. At this time, information on the IP and a synopsis of the protocol is usually available and provides you enough information to conduct the preliminary stage. Based on the profile of the IP, is it safe and suitable for administration? Is the targeted patient population available? If yes, does it support the proposed enrollment rate? Should private or public clinical sites be favored? Should a centralized or local laboratory be used? Did investigators have negative and/or positive comments regarding the study design? What are the identified risks? All of these questions must be answered before we can move on to the next stage. Based on the answers to these questions, any necessary modifications must be made to the planned study. This preliminary stage is the most critical one and yet often the most overlooked in clinical trial management for an array of different reasons. For example, some may not think it is necessary due to previous experiences, have recently done a similar study, or because they feel it can be done at a later stage in the study. Many of the logistical challenges commonly encountered in clinical trial management can be identified and resolved at this stage.If the preliminary stage indicates that the project is feasible, we can move on to the next stage. If not, the project should be carefully analysed and either modified or cancelled altogether. - Initiation stage:
Based on the valuable information gained during the preliminary stage, the initiation stage is really where the clinical trial project is shaped and fine-tuned to maximize a positive outcome. It must address the “Why” and the “What” portions of the trial project, prepare for any possible challenges, and set the required capital (human, financial and material) and study timelines. Regarding timelines, three scenario schemes should be prepared – the worst case, the realistic, and the best case scenarios. It would also be highly recommended to set aside a contingency budget to take into consideration the worst case scenario timeline as it usually translates into additional costs. The protocol should be finalized at this point, regulatory/ethical questions should be solved, and potential clinical sites should at least be identified and their capabilities validated. The logistical aspects of the study should be clear and well-defined by the end of the initiation stage. - Planning stage:
Planning is the third stage of clinical trial management when applying the PMBOK system and if the “Preliminary” and “Initiation” stages were well conducted, the Planning stage will be relatively straightforward. This stage must answer the “How” portion of the trial project. This means creating and putting together the roadmap (including the processes) that will enable you to fulfill the total scope and objective(s) of the study. For example, you can now determine which IRB will be used, as well as when and who will be completing the submissions. The final sites will be selected for the study, and all standards and processes for communication during the study will be well established. The processes for recruitment of patients and clinical monitoring of sites, and all logistical aspects of the investigator meeting, the investigational product shipment, randomization, data management and archiving will be completely defined during this stage. Unfortunately, the planning stage is often where both experienced and less experienced clinical trial management teams first begin their work on the study, instead of going through the Preliminary and Initiation stages first. If the first two stages are skipped, it is very likely that various challenges will arise throughout the trial that will cause the project to exceed budgets, timelines, or even result in termination of the study. In order to effectively plan a study, the “Preliminary” and “Initiation” stages must be fully executed beforehand. Overall, the Planning stage involves the finalization of all aspects of the trial in order to actively start the engine of the project and get it rolling. - Execution stage:
The trial is now up and running and the “Execution” stage consists of following the roadmap which was prepared in the “Planning” phase, and abiding by all study requirements and schedules. - Tracking and Controlling stage:
Both the “Execution” and “Tracking and Controlling” stages are to be performed simultaneously in order to ensure quality of execution and that prompt actions will be taken to resolve any issues that arise during the execution of the trial. If we were driving a car, the accelerator pedal would represent the execution stage, and the brake pedal the tracking and controlling stage. Ensuring that appropriate metrics, communication and other systems are in place to provide constant feedback will enable proper tracking of the study. - Closing stage:
In most cases, a clinical trial project is considered to be closed once the final report has been completed. During the closing stage, the core study team, including the sponsor, clinical sites and vendors, should engage in an overall evaluation session to have a transparent and constructive discussion of the completed trial project (i.e. a “lessons learned” session). This allows for a thorough evaluation of the overall trial management performance, including an assessment of whether the study objectives were achieved as planned and a discussion of the study highlights (good and bad), challenges and applied solutions. The main goal of the closing stage is to constantly improve trial management skills from one project to the next.
- Preliminary stage:
 Making the best of problematic situations
Making the best of problematic situations
Despite my many years in the clinical trial arena, I have yet to see “the perfect study”, and despite the best preparations and proactive strategies applied in clinical trial management, problematic situations can still arise. Fortunately, there are many methods that can be used to tackle these issues, with the most common being Corrective Action Preventive Action (CAPA) and Root Cause Analysis. If time is limited, a rule of thumb principle to rapidly identify a root cause of any issue is the “5 Whys” iterative questioning technique[3]. By asking the question “Why?” after each provided response regarding an issue, the fifth response should be a probable root cause. For example, if you are noticing an increase in protocol deviations at a site, the “5 Whys” process may proceed as follows:
Problem statement: A significant increase in protocol deviations at a clinical site over the last 30 days.
- Why has there been an increase in protocol deviations lately? (First Why)
– Because we have to work faster. - Why do you have to work faster? (Second Why)
– Because we’ve been very busy lately. - Why have you been busy lately? (Third Why)
– Because we are behind schedule for multiple projects and are trying to catch up. - Why are you behind schedule? (Fourth Why)
– Because we now have only 2 study coordinators instead of 4. - Why do you now have only 2 study coordinators? (Fifth Why)
– Because the other 2 coordinators are on vacation. (Probable root cause)
- Why has there been an increase in protocol deviations lately? (First Why)
Another effective tool in making the best of problematic situations is ensuring that excellent two-way communication exists with all stakeholders – mainly the clinical sites since they are at the forefront of conducting the trial. Clinical sites are usually the first to identify or experience problems and should therefore report it to the clinical trial management team promptly. This enables the clinical trial management team to resolve the problem in collaboration with concerned stakeholders as soon as possible in order to prevent the issue from worsening or possibly spreading to other sites.
When a problem arises, the goal is not to point fingers and blame someone, but to come up with possible solutions and apply the most effective one using a cooperative team approach.
Project management best practices are being recognized across many industries as a valued driver for increased organization in the workplace, leading to process excellence and optimization. Globally, Sponsors and CROs are seeing the immense benefits of adopting the PMBOK principles on their clinical trial management performance.
About the Author
Reginald Exume, Scientific Project Manager at Vantage BioTrials, Inc. With over 14 years of clinical research experience in the generic and innovator pharmaceutical industry, Reginald is a professional with an excellent overview of both the management and scientific aspects of drug and clinical development.
References:
- Project Management Institute
- PMBOK Guide, 4th Edition, Project Management Institute, 2008
- iSixSigma, “Determine the Root Cause: 5 Whys”